Wireless Device To Provide New Options For Colorectal Cancer Treatment

For those diagnosed with colorectal cancer, surgery has been the only option that offers a solution. Unfortunately, surgery is frequently complicated by disease recurrence at the site of the original cancer when microscopic cancer cells are left behind at the time of surgery. Chemotherapy is a treatment option that is often given in conjunction with surgery, although it can lead to toxic side effects.
Sung II Park, assistant professor in the Department of Electrical and Computer Engineering and researcher in the Center for Remote Health Technologies and Systems at Texas A&M University, and his team are working to develop a low cost, minimally invasive wireless device that offers precise, safe treatment options for cancers.
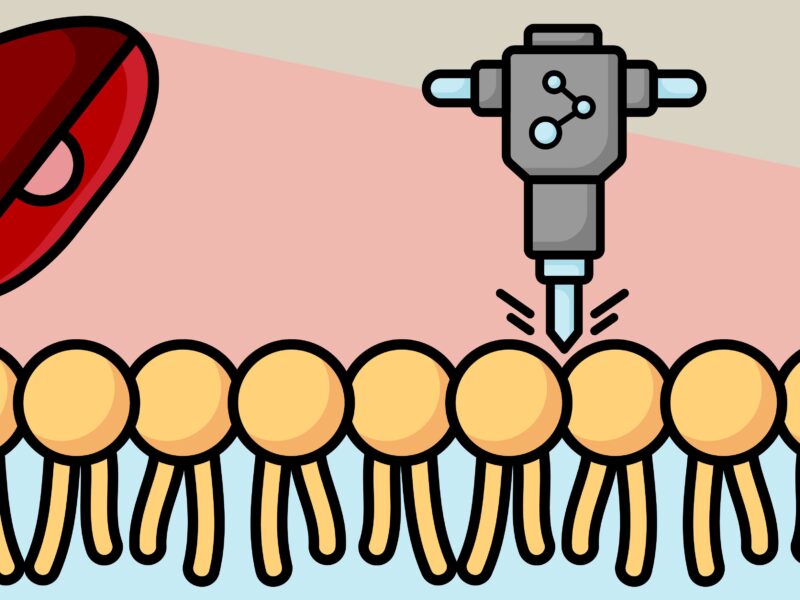
The researchers will utilize photodynamic therapy (PDT) during surgery by using a photosensitizer — a drug activated by light — to kill the cancer cells. During this process, surgeons will be able to remove the bulk of the tumor, then fully irradiate the tumor bed when the photosensitizer is activated by the light. This combination would result in a complete treatment in a safe and effective way with no toxic side effects.
“The biocompatible, miniaturized implantable LED device will enable light dosing and PDT that is tailored to the individual tumor response,” Park said.
In the long term, the work will result in a platform that has the potential to provide clinical-quality health monitoring capabilities for continuous use beyond the confines of traditional hospital or laboratory facilities; it will also allow for treatment options to prevent the development of additional malignancy and therefore significantly improve the quality of life for people with cancer. This type of platform would also reduce the huge economic burden on oncology resources, which totaled $167 billion U.S. dollars in 2020 alone. In 2022, projected global oncology spending will reach $206 billion, a 23.35 percent increase.
Further details about their device are published in the April issue of Nature Communications.
Excluding skin cancers, colorectal cancer is the third most common cancer worldwide, according to the American Institute for Cancer Research. According to the American Cancer Society, this year, an estimated 149,500 adults in the United States will be diagnosed with colorectal cancer and it’s expected to cause about 52,980 deaths.
Although photodynamic therapy has been shown to be effective in many solid tumor cancers, its clinical application has been limited by an incomplete understanding of the differing response of cancer and normal tissue, and a lack of methods to monitor tumor response and adjust light dosage accordingly.
To address this gap, Park and his team have proposed a two-step procedure. First, the photosensitizer drug is administered, which is preferentially taken up by the tumor cells, and then the tumor is illuminated by non-thermal light at a wavelength that matches an absorption spectrum of the drug. Activation of the drug induces a photochemical reaction that triggers tumor cell death.
“The intracavity device will provide a minimally invasive, biocompatible platform for light detection of residual cancers and delivery to tumor cells located in any part of the body, suggesting it could make an impact in the areas of breast, kidney, lung, pancreatic, prostate, ovarian and rare cancers,” Park said.
Other contributors to the research include several well-known researchers from the electrical and computer engineering department, the University of Leeds and Sun Moon University.
This work was supported by grants from the interdisciplinary X-Grants Program, part of the President’s Excellence Fund at Texas A&M, the 2018 National Alliance for Research on Schizophrenia and Depression Young Investigator Awards from the Brain and Behavior Research Foundation and the Precise Advanced Technologies and Health Systems for Underserved Populations Engineering Research Center. This work was also supported by a Wellcome Trust Institutional Strategic Support Fund Fellowship, a National Institute for Health Research (NIHR) Research Professorship and an NIHR Senior Investigator Award.
This article by Rachel Rose originally appeared on the College of Engineering website.