Texas A&M Professor Awarded Department Of Defense Grant For Gulf War Illness Research

Thousands of American troops who were deployed in the First Gulf War were exposed to a variety of chemicals that resulted in psychological and physiological symptoms that health experts call Gulf War illness (GWI), previously called Gulf War syndrome.
Ashok Shetty, professor in the Department of Molecular and Cellular Medicine and associate director for the Institute for Regenerative Medicine at the Texas A&M University College of Medicine, has teamed up with Kimberly Sullivan from the Boston University School of Public Health and Dr. Nancy Klimas Nova Southeastern University to investigate the extent and mechanisms of brain inflammation in veterans with GWI through a liquid biopsy approach. Their research efforts are being funded by a $1 million grant from the Department of Defense (DOD) over a three-year period.
The condition is characterized by a collection of unexplained chronic symptoms that can include gastrointestinal problems and dermatitis (a skin disorder) or central nervous system problems such as cognitive dysfunction, neuroinflammation, memory problems and depression. Nearly 30% of Gulf War veterans suffer from chronic GWI. Currently, the mechanisms underlying these persistent issues are unknown.
Shetty’s earlier studies on GWI focused on the animal model of GWI, recreating the conditions and chemicals veterans were exposed to during the war. He found that the animal models developed cognitive problems and had increased behavior that was associated with inflammation in the brain. His studies showed that the neuroinflammation in the brains of the animal models was progressive and had gotten worse over time, which explains why GWI is still prevalent in Gulf War veterans 30 years after the war.
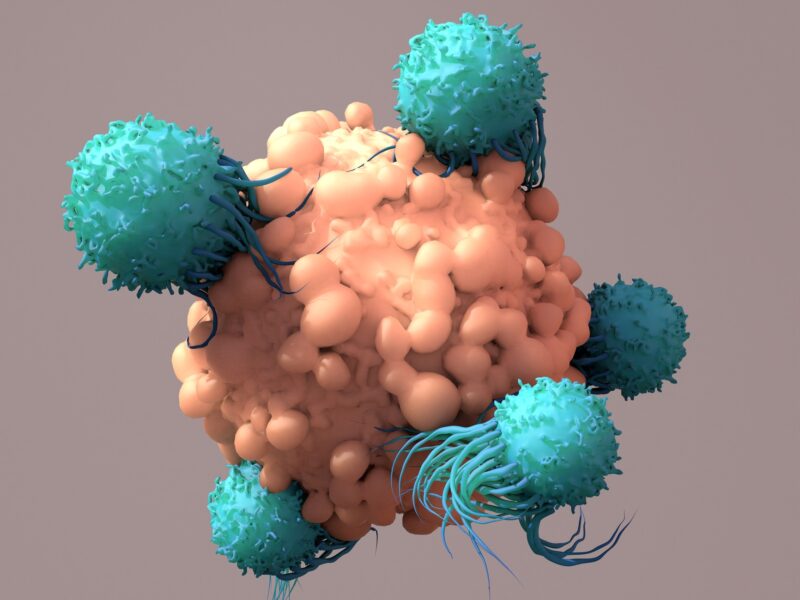
Compared to an animal model approach, studying the brain in veterans with GWI is difficult. Therefore, most research with humans has been done through blood sampling, but it’s difficult to see if the results actually reflected what was happening in the brain. As a result, Shetty developed a liquid biopsy approach, which involves the characterization of the composition of “brain-derived extracellular vesicles” in the blood.
Shetty and his team will use this liquid biopsy approach to study neuroinflammation in the blood of Gulf War veterans beginning in early 2021.
The Sullivan and Klimas laboratories will collect blood samples of 50 veterans with GWI (patients) and 50 veterans without GWI (controls). Once the blood samples are collected, they will send the samples to Shetty’s laboratory. Shetty will then use the blood samples to isolate the extracellular vesicles (EV) — membrane-enclosed nanosized vesicles that carry cargo such as proteins, lipids and micro-RNAs — that come from the brain.
Once the extracellular vesicles are isolated, he will classify each one as a neuron-derived extracellular vesicle (NDEVs) or an astrocyte-derived extracellular vesicle (ADEVs) using a specific tagging technology. Then, Shetty will examine the cargo in the NDEVs and ADEVs, particularly proinflammatory mediators and microRNAs using biochemical assays and RNA sequencing.
“Because the composition of EVs reflects the physiological or pathological state of cells from which they are derived at the time of secretion, analysis of EVs derived from specific brain cells in the blood would help in the identification of biomarkers linked to chronic brain impairments,” Shetty said.
What this approach means is by just looking at the vesicles, one can tell what is going on in the brain, even the brain cannot be directly studies. This technique of isolating extracellular vesicles was developed by Shetty in 2019, when he used an animal model approach.
“Whatever is happening in the brain can be determined by characterizing brain-derived vesicles in the blood,” Shetty said. “It can be neuron-derived vesicles and astrocyte-derived vesicles, so this project is about that. But now, instead of animal models, we are studying actual veterans. From this human study, we can identify the extent of neuroinflammation in veterans.”
Ultimately, this study will likely provide evidence as to why GWI is worse for some veterans compared to others, help diagnose the extent of brain inflammation in veterans with GWI and help determine whether GWI puts veterans at a higher risk for developing other neurological diseases.
“The approach is also efficient in future clinical trials for monitoring the remission or progression of brain inflammation with apt treatment strategies,” Shetty said.
This article by Gracie Blackwell originally appeared on Vital Record.