Could Stem Cells Be Used To Treat COVID-19?
While the medical community continues working to find treatments and a vaccine for COVID-19, a Texas A&M University regenerative medicine researcher says results from clinical trials for stem cell therapy indicate that it could be a safe and efficient way to treat the sickest patients.
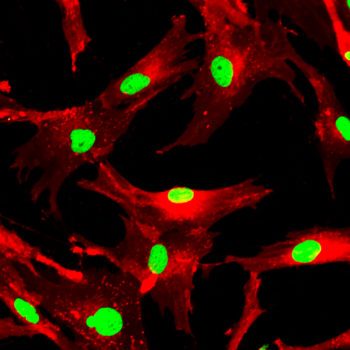
Mesenchymal stem cells — which can be found in bone marrow, adipose tissue, placentas and umbilical cords — are known to regulate the immune system in a variety of disease models when isolated from donors and infused intravenously in patients. Ashok K. Shetty, associate director of the Institute for Regenerative Medicine, said clinical trials with promising results suggest that mesenchymal stem cells (MSC) may help treat COVID-19 patients who develop complications like acute respiratory distress syndrome (ARDS) or cytokine release syndrome induced by ARDS.
“Based on the studies it looks really promising, particularly for COVID-19 patients who develop complications, like ARDS, or a humungous elevation of pro-inflammatory cytokines or pneumonia,” Shetty said.
A response observed in patients with severe cases of COVID-19, the disease caused by the novel SARS-CoV-2 coronavirus, is hyperactivation of the immune system known as cytokine release syndrome, or a “cytokine storm.” Shetty said this occurs when the immune system kicks into overdrive, and the resulting inflammatory reaction can damage the patient’s tissue and organs.
He said several trials are examining the use of MSCs for ARDS, which is a build-up of fluid in the lungs that results in oxygen deprivation. COVID-19 patients with ARDS symptoms are placed on ventilators, Shetty said. It’s a common manifestation of cytokine storms, and the cause of death for many patients.
Shetty points to a recent study in China that showed MSCs can help combat a cytokine storm. Seven COVID-19 patients who received intravenous infusions of MSCs all had better outcomes with MSC infusions than with the standard treatment, he said. While that research has been criticized for the small number of patients, Shetty said results from hundreds of patients from other clinical trials will likely be forthcoming in three to four weeks.
Shetty, who is also a professor in the Department of Molecular and Cellular Medicine, is co-editor-in-chief of Aging & Disease, the journal that published the Chinese study.
“It is more effective for patients who develop complications. That’s because we want to suppress the over-activation of the immune system, but you do not want to suppress the initial activation of the immune system that’s really required for reducing the viral load,” Shetty said. “So, too-early administration may not be helpful. But for those patients who develop complications and need to get on the ventilators, those are the ideal candidates for MSC therapy, in my opinion.”
The presentation of the disease has shown to vary widely between infected individuals. While some people may show no symptoms or experience a flu-like illness that can be treated at home, some patients become critically ill with upper respiratory complications like pneumonia. More than 248,000 people have died from COVID-19 worldwide, and more than 3.5 million positive cases have been confirmed over the course of the pandemic.
The U.S. Food and Drug Administration has not approved wide-scale clinical trials for MSCs, but on April 5 it approved MSC treatments for patients with a poor prognosis. Doctors at the University of Miami and the University of Texas Health Science Center at Houston have both received emergency Investigational New Drug (IND) approval from the FDA for infusion of different sources of donor MSCs in COVID-19 patients.
“Safety has been established for MSC infusions in human trials,” Shetty said. “It’s probably very useful in saving lives, because people on ventilators do not have an efficient treatment right now. All kinds of drugs are being tried, but the efficacy is still unknown.”
Media contact: Caitlin Clark, caitlinclark@tamu.edu