The Opioid Epidemic In Our Backyard: Health Science Center Offers Policy Solutions
Highlights
- The opioid crisis costs an estimated $78.5 billion annually
- Forecasts predict an annual death toll increase by at least 35 percent from 2015 to 2027
- College of Pharmacy professor Juan F. Castro: “It is up to each one of us, individually as physicians, not to cross that thin clinical and ethical gray zone of providing comfort for our patients or inducing an addictive disease in a patient.”
Even though the federal government declared opioid abuse a national emergency, experts are still trying to figure out a comprehensive solution to this crisis. From 1999 until 2015, more than 183,000 people in the United States died from prescription opioid-related overdoses. Since 1999, overdoses due to this class of drug have quadrupled, according to the Centers for Disease Control and Prevention (CDC).
Eric Grayson, PharmD, clinical assistant professor of pharmacy practice at Texas A&M Irma Lerma Rangel College of Pharmacy, held panel presentations to illustrate how an interdisciplinary approach—one involving medical and pharmacy professionals, along with elected officials and law enforcement officers—is necessary to address the opioid epidemic.
“This problem has plagued practitioners for a long time. Too many people are dying, and we need a more comprehensive approach,” Grayson said. “Medicine, pharmacy, enforcement, regulatory and treatment practices, along with social and cultural influences, all play a part in solving the central issue of this crisis, opioid use disorder.”
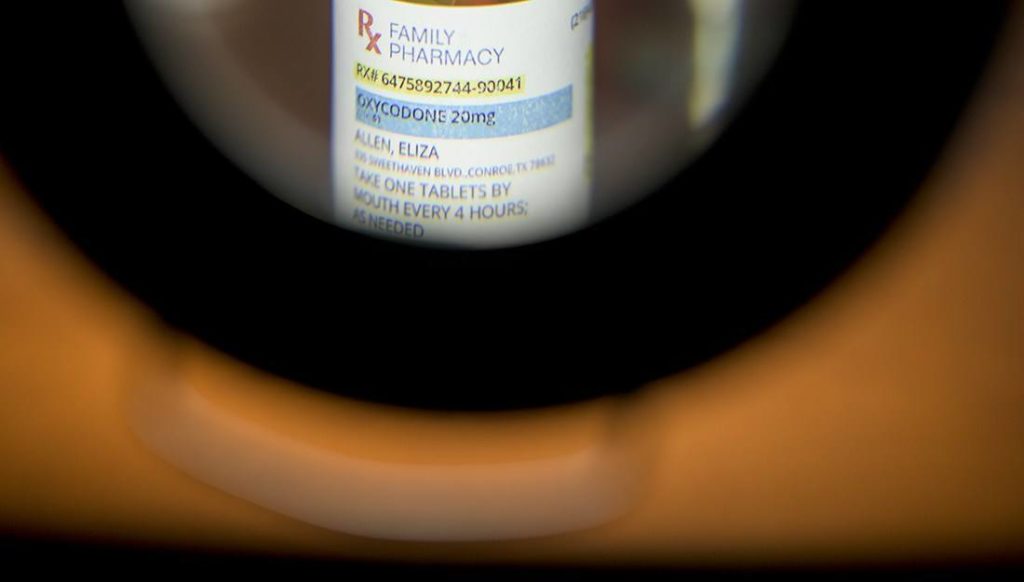
Grayson recalled a time when opioids were considered unsafe for chronic pain, due to the risk of addiction. However, when OxyContin entered the marketplace in 1995, a New England Journal of Medicine study from 1980 received hundreds of citations from those lobbying for this long-acting opioid pain medication. This study reported that addiction is rare in patients treated with opiates for acute surgical pain. Although OxyContin was being marketed for chronic pain, this study was used to justify its safety regarding addiction. Grayson believes that excessive prescribing of OxyContin is the nucleus of opioid abuse. Today, the opioid crisis costs an estimated $78.5 billion annually, including health care, criminal justice involvement and lost productivity.
The effects of opioid abuse
Juan F. Castro, MD, assistant professor and interim vice chair of pharmacy practice at Rangel College of Pharmacy was a speaker at the panel presentations. “As a primary care physician, I have seen multiple effects of opioids abuse,” Castro said. “Clinically, the number of narcotic prescriptions issued in primary care has decreased as fewer doctors are writing these prescriptions, and the doctors who continue to prescribe them are more careful with which patients receive them. In the nonclinical setting, clinicians are concerned not only about government penalization for over-prescription but also of some patients committing violent acts when opioids are not prescribed. This crisis has reached a point where nationwide, several doctors have been physically hurt or killed by desperate patients seeking opioids.”
Opioid Crisis Leads To Abuse Of An Unusual Suspect: Antidiarrheal Medication
Even as physicians try to be more careful, knowing when and how much pain control patients need is not always black and white. “There is a collateral effect for patients needing appropriate pain control,” Castro said. “In being cautious not to over prescribe, at times some patients who would legitimately benefit from opioids, such as those in surgical pain, are not receiving medication to appropriately deal with the pain. We are trained to stay away from actions or drugs that cause harm. That’s part of our oath: First do no harm. But our nature and training are also to alleviate pain. It is up to each one of us, individually as physicians, not to cross that thin clinical and ethical gray zone of providing comfort for our patients or inducing an addictive disease in a patient.”
In June 2017, STAT News forecasted that opioids could kill nearly half a million Americans in a decade, as the addiction and overdose problem exacerbates. Forecasts predict an annual death toll increase by at least 35 percent from 2015 to 2027, with the gravest scenario depicting more than 93,000 deaths annually. Fatal overdoses in these models do not level off until after 2020, as it will take time to assess if federal drug enforcement efforts and recommendations to doctors for prescribing fewer opioid pills are going to be effective.
Identifying abusers
Two students at the college, Khoi Vo and Andy Wong, looked into practical regulatory solutions to opioid abuse as part of the panel presentations. They assessed the effectiveness of prescription monitoring programs (PMPs), which are programs through state agencies that collect and monitor prescription data for controlled substances dispensed by pharmacies.
“A PMP is a vital tool to combat the opioid crisis. PMP checks for doctor and pharmacy shopping, identifying patients who may be abusing or diverting their drugs; this database can be used by pharmacists and prescribers,” Wong said. “There are 34 states mandating that prescribers, pharmacists or both submit PMP queries, and early efficacy studies show decreased usage of opioid volume.”
Texas recently passed a law mandating use of a PMP. House Bill 2561 passed on June 9, 2017, to amend Texas Controlled Substances Act. Starting September 1, 2019, registered pharmacists are required to access the state PMP before dispensing opioids.
CDC recommends that physicians consider alternatives to opioids, and if they must be used, the lowest possible dosage be prescribed, alongside close monitoring of patients. PMP enables identification of those who are “doctor and/or pharmacy shopping,” meaning purchasing vast quantities of controlled substances through numerous doctors or pharmacies, and are therefore at a far higher risk of overdose. The CDC recommends a linkup of electronic health records so that the information is well integrated into health care providers’ daily practices.
“It’s going to take the whole team to solve this,” Grayson said. “If we take these products off the street and make fewer drugs available, lives are saved. That is clearly shown in the data from states where enforcement has had an impact on the availability of illegal prescription drugs. We can ask prescribers and dispensers to check the PMP before dispensing, which also is shown to decrease the number of prescription opioid deaths. There are trend lines on that in the literature. If we all do this together, the end result would be an improvement. If one part of the team does not work in concert with everyone else, we are just moving the problem around.”
###
This story by Tamim Choudhury originally appeared in Vital Record.