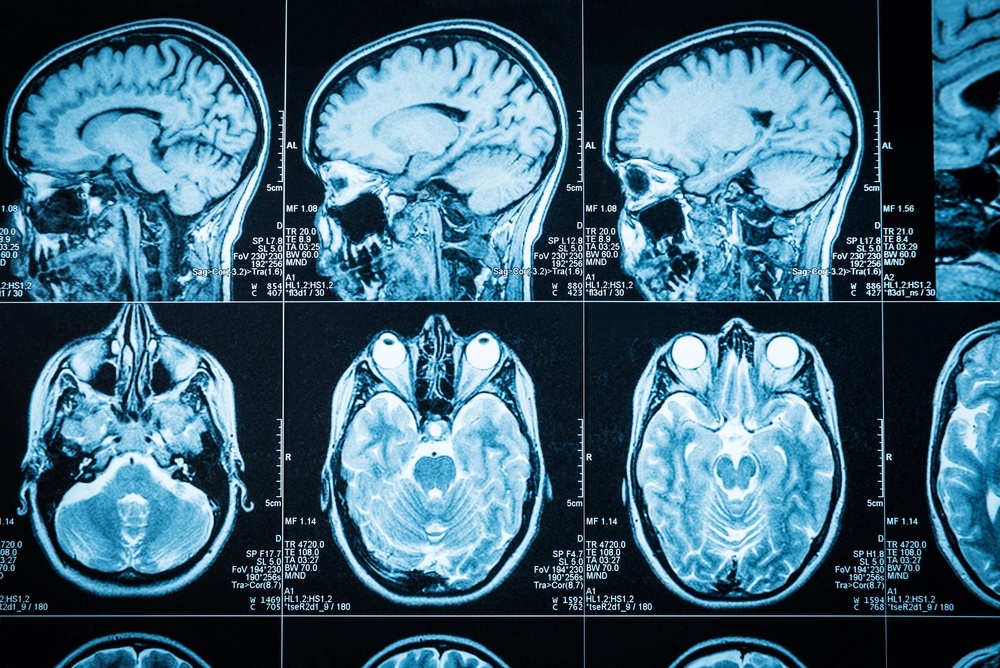
Despite several clinical trials of various therapeutic strategies, there are currently no drugs for curing or preventing epilepsy and few promising ones in the pipeline. Antiepileptic drugs are the lifeblood for symptomatic treatment of seizures, but these medications do not significantly affect the problem underlying epileptogenesis, which is when a normal brain becomes progressively epileptic over a period of months or years.
Texas A&M researchers are changing this landscape by designing next-generation epigenetic therapies, which are small-molecule drugs named for their ability to alter gene expression by targeting what are called epigenetic regulators. These medications could be a new frontier to combat a variety of diseases, like cancer and epilepsy, that are marked by abnormal gene expression.
Although many such strategies are under investigation to verify the potential impact of epigenetic therapies, D. Samba Reddy, PhD, RPh, professor & National Institutes of Health CounterACT investigator in the Department of Neuroscience and Experimental Therapeutics at the Texas A&M College of Medicine, has found a new molecule, called histone deacetylation (HDAC), as critical target for epigenetic interruption of epileptogenesis. This strategy was explained in a recent paper Reddy published in the journal Pharmacology & Therapeutics, along with co-author Iyan Younus of Cornell University.
“We found for the first time that selective inhibition of HDAC by experimental drugs not only retards the progression of epileptogenesis, but even reverses the epileptogenic state in validated models used by the U.S. Food and Drug Administration to approve drugs for treatment of epilepsy,” Reddy said. “Since HDAC inhibition provides long-term protection against epileptogenesis, the epigenetic HDAC pathway represents a novel target for anti-epileptogenic or disease-modification therapy in the challenge of preventing and curing epilepsy.”
https://today.tamu.edu/2016/10/26/alcoholism-research-a-virus-could-manipulate-neurons-to-reduce-the-desire-to-drink/
Epilepsy is a chronic brain disease characterized by repeated unprovoked seizures, which can sometimes even lead to death. Epilepsy affects nearly 3 million people in the United States and 65 million people worldwide. About 150,000 new cases of epilepsy are diagnosed in the United States each year. Unfortunately, other than surgery, there is currently no therapy option for curing epilepsy or preventing its onset in people at risk.
Epilepsy development is complex and irreversible process that can be described in three stages: the initial epileptogenic event, the latent period with little or no seizure activity and the chronic period characterized by recurrent seizures. Many treatments targeting different pathways have been studied, but antiepileptic medications haven’t been able to stop this process from continuing to the chronic stage. That’s where epigenetic regulators come in.
“We are one of few labs in the world to harness the power of epigenetic tools to enable powerful new strategies to treat or prevent the development of epilepsy in people at high risk for this disease, like people afflicted by traumatic brain injury, meningitis, stroke, chemical neurotoxicity or drug withdrawal seizures,” Reddy said. “Epigenetic intervention appears a rational strategy for preventing epilepsy because it targets the primary pathway that initially triggers the numerous downstream neuronal events mediating epileptogenesis.”
Epigenetic drugs fall into three main categories: writers, erasers and readers. Writers modify a type of protein called histones by adding certain groups that result in acetylation or other modifications, while erasers remove such groups. These changes are recognized by readers that ultimately enable regulation of gene expression by changing the structure or configuration of the materials that make up chromosomes.
Histone acetylation and deacetylation controls the activation of whether genes are turned into proteins or not. Thus, modulating of the extent of HDAC activity provides a best strategy to prevent pathological progression. Many HDAC inhibitors are currently being used in clinical trials for cancer and other diseases. The epigenetic strategy has many advantages, including a wide availability of clinically-approved HDAC inhibitors, a concrete strategy based on the pathogenic mechanism and the potential for preventative, long-term protection rather than symptomatic treatment.
“To truly harness the power of epigenetic therapies, researchers need a thorough knowledge of epigenetic mechanisms,” Reddy said. “This approach, however, although still requiring further study including clinical trials, is broader than typical antiseizure treatments and represents a mechanistic strategy for preventing epilepsy.”
Reddy’s team is collaborating with the Texas A&M Center for Epigenetics & Disease Prevention in Houston and has received a grant from the United States Department of Defense.
###
This story by Christina Sumners originally appeared in Vital Record.