Repairing Bones With Stem Cells
When you break a bone, you get a cast, and in a few weeks or months, your fracture heals. But what happens when the injury is so severe that the bone can’t knit itself back together? Or when the patient has osteoporosis, diabetes or another condition that impairs bones’ healing ability? If you are lucky, you might have a metal rod implanted that helps hold everything together, but in severe cases, people can lose limbs.
Researchers at Texas A&M are trying to find a better way.
Carl Gregory, Ph.D., an associate professor in the Institute for Regenerative Medicine (IRM) at the Texas A&M Health Science Center College of Medicine, is working on using mesenchymal stem cells (MSCs) to heal bones faster and more effectively.
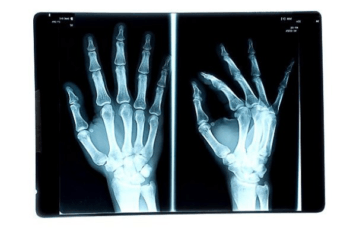
MSCs are not the same as the embryonic stem cells that are the source of so much controversy. Instead, MSCs primarily come from adult bone marrow and fat tissue. They form a number of types of connective tissue, and when they are injected at the site of a bone injury, they can (in theory, at least) change, or differentiate, into the cells that repair bones.
However, the studies testing this in live animals haven’t worked as well as researchers had hoped.
“It’s taken us quite a while to discover why these cells do so well in the dish, but they don’t do well in animal models,” said Gregory, who joined the Texas A&M Health Science Center in 2008. Although about two teaspoons of adult bone marrow can be cultured into millions of cells, the process is very complicated: the cells have to be grown correctly and primed in such a way that they know they are going to become a bone-producing cell. At the same time, if a cell is primed too much, it dies rapidly after it is put into the body.
Even when all of this is done correctly, the cells tend to disappear after a few weeks at the site of the bone fracture. “The body will only invest a certain amount of time to bridge a bone injury with new tissue, usually around two weeks for a small animal, and a bit longer for a person. If this process fails, the injury will not heal.” Gregory said. To extend this time, he and his biomedical and electrical engineering colleagues in the Texas A&M Dwight Look College of Engineering are developing a way to inject the cells, along with an accompanying “biomatrix,” to the injured area. This biomatrix is essentially a mix of proteins that make up young bone tissue, and research done by Gregory and his team and supported, in part, by the National Institutes of Health (NIH), has shown that the matrix can help the cells stay put and create a living, bone-like construct. The engineers are now working on better ways, including nanotechnologies, to deliver the cells and the matrix.
Continue reading on Vital Record.
This article by Christina Sumners originally appeared in Vital Record.