Highlights
- A Texas A&M psychiatry professor helped lead the Department of Veterans Affairs study
- The study’s results showed a significantly greater likelihood of near complete relief of depressive symptoms during the 12-week acute treatment phase
- Major depressive disorder affects an estimated 13 to 14 million American adults
A clinical trial from Department of Veterans Affairs (VA) of veterans with major depressive disorder, published this month in the Journal of the American Medical Association (JAMA), found that the addition of an atypical antipsychotic medication to an antidepressant regimen showed greater improvement in symptoms of depression than switching to another antidepressant among patients who were not responding to their current antidepressant treatment.
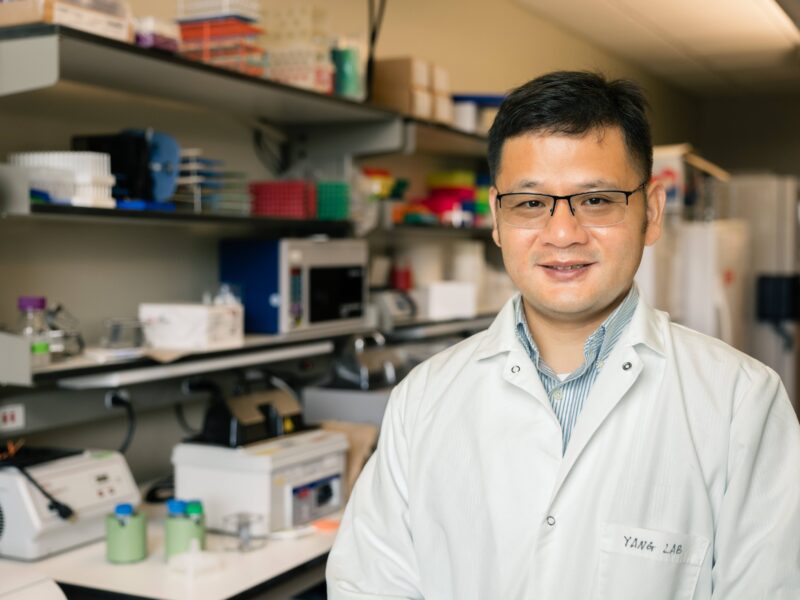
“This is the largest study ever performed of ‘next-step’ pharmacotherapy for patients who did not have an adequate response to initial antidepressant pharmacotherapy,” said Paul B. Hicks, MD, PhD, vice dean and professor of psychiatry and behavioral sciences at the Texas A&M College of Medicine in Temple and one of 12 people on the study’s executive committee. “This is the best and largest comparison of switching versus augmentation strategies for ‘next-step’ pharmacotherapy that has been published. This study looks at the safety and efficacy of the use of a second-generation antipsychotic as an augmentation strategy for treatment-resistant depression.”
Hicks served as the initial site investigator for the Central Texas Veterans Health Care System, one of 35 VA medical centers across the country participating in the research, but was replaced in this role by Solomon Williams, MBBS, assistant professor of psychiatry and behavioral science, when Hicks became vice dean for the Temple Campus. The study’s executive committee, which provided oversight for the implementation of the project, including key decisions about management of the project from its inception until data analysis, also included principal investigators Somaia Mohamed, MD, PhD, of the VA New England Mental Illness, Research, Education, and Clinical Center and Yale Medical School, and Sidney Zisook, MD, VA San Diego Healthcare System and University of California, San Diego. Mohamed, a neuropsychologist, is a former associate professor in the Texas A&M College of Medicine Department of Psychiatry and Behavioral Science.
Opioid Crisis Leads To Abuse Of An Unusual Suspect: Antidiarrheal Medication
“Failure of depression pharmacotherapy is a major public health problem affecting millions of Americans each year,” Mohamed said. “There is a tremendous need for evidence on which treatments work best for these patients, and we found that among the three strategies evaluated in this study, evidence of the greatest symptom benefit was provided by adding an antipsychotic to previous antidepressant therapy.”
Major depressive disorder is a chronic, disabling disorder that affects an estimated 13 to 14 million American adults, or 5 percent of the adult population, annually. Previous large studies have shown that fewer than one-third of patients achieve remission with their first course of antidepressant pharmacotherapy. Thus, each year, as many as 9 million Americans may need a new treatment for their depression. A treatment that helps only 1 percent of these patients reduce depressive symptoms more than commonly used alternatives could potentially bring important relief to almost 100,000 Americans annually. Past studies have also compared treatments commonly used as “next step” therapies in major depressive disorder, but found no treatment to be significantly more effective than others.
However, since 2007, several antipsychotic medications have been approved by the US Food and Drug Administration (FDA) to be used in addition to antidepressant medication for patients whose depression has not responded to antidepressant treatment alone. Antipsychotic augmentation therapy has been found to be more effective than a placebo, but until now, no large study has compared it to other approved antidepressant switching or augmentation strategies.
###
Continue reading this story by Christina Sumners on Vital Record.