How Cancer Cells Escape From The Immune System
Under normal circumstances, the immune system recognizes and successfully fights cancer cells, eliminating them as they develop. However, sometimes the process breaks down and tumors form, and now we know why. Researchers at the Texas A&M Health Science Center found that when cancer cells are able to block the function of a gene called NLRC5, they are able to evade the immune system and proliferate, according to research published today in the Proceedings of the National Academy of Sciences (PNAS).
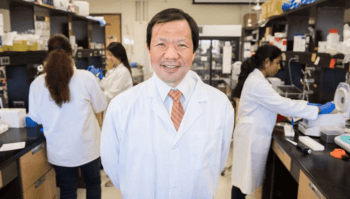
“We found the major mechanism of how cancer cells escape from our immune system and form tumors,” said Koichi Kobayashi, M.D., Ph.D., professor at the Texas A&M College of Medicine and a lead author on the PNAS article. The discovery indicates NLRC5 as a novel biomarker for cancer patient survival and therapeutic response, as well as a potential target for new treatments.
“Cancer cells are born because of genetic changes, such as mutations or rearrangement of pieces of different chromosomes,” Kobayashi said. “Because of this, all cancer cells have new, ‘foreign’ genes, which host T-cells generally detect as tumor antigens. This anti-tumor system works very well.”
Kobayashi and his colleagues discovered several years ago that NLRC5 regulates major histocompatibility complex (MHC) class I genes. These genes code for molecules on the surface of cells that present fragments of foreign proteins—such as those from a virus or bacterium— that have invaded the cell. These fragments notify a part of the immune system called cytotoxic T cells, triggering an immediate response from the immune system against that particular foreign antigen.
The novel finding in this study is that the same system should work to destroy cancer cells, but sometimes they find a way to disable the NLRC5 gene, thus enabling them to evade the immune system and form tumors.
“If MHC class I antigen presentation does not work, cancer cells will not be killed by T cells,” said Sayuri Yoshihama, M.D., Ph.D., a fellow in Kobayashi’s lab and first author of the paper. “We found that function and expression of NLRC5 is reduced in cancer cells by various mechanisms, and the result is immune evasion by cancer cells.”
In fact, based on biopsy samples from 7,747 solid cancer patients in The Cancer Genome Atlas (TCGA) database, expression of this NLRC5 gene is highly correlated with cancer patient survival in various cancer types—especially melanoma, rectal cancer, bladder cancer, cervical cancer and head/neck cancer—with patients who survive longer tending to have greater expression of NLRC5. Among these, melanoma and bladder cancer displayed the most striking differences, with 5-year survival rates of 36 percent and 34 percent in the NLRC5-low expression group compared with 71 percent and 62 percent in the NLRC5-high expression group, respectively.
“With this finding of NLRC5 as an important biomarker for cancer, we can ultimately predict how long cancer patients can survive and how well cancer treatments might work for them,” Kobayashi said. It might be especially relevant for melanoma patients, both because NLRC5 mutation rate is relatively high and because its levels of expression are highly predictive of survival for that cancer type.
Continue reading on Vital Record.
This article by Christina Sumners originally appeared in Vital Record.