Is 3D Printing The Future Of Drug Manufacturing?
Grey’s Anatomy fans may remember the plotline that had Meredith Grey using a 3D printer to try to create portal veins. Although real medicine isn’t quite there yet, health care professionals can use the technology to produce medication.
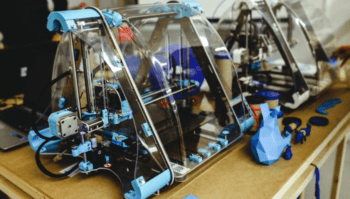
3D printing works by applying layer upon layer of a substance until the shape, thickness and volume you want is created. In this case, to create a pharmaceutical tablet, each layer of drug would be alternated with a layer of “glue” to hold it all together, and each pill would have exactly the amount of drug required. This ability to create a product, one at a time, layer by layer, can greatly expand the potential of precision medicine, and perhaps the place it is most useful is in pediatric medicine.
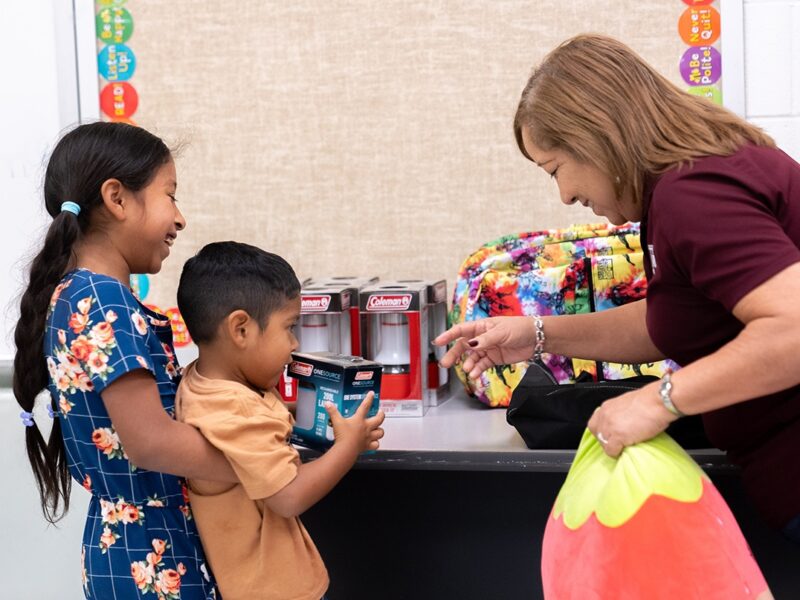
Giving the correct dose of a drug to children is notoriously difficult. Their small size, combined with metabolic factors that make medications behave differently in pediatric patients, can create any number of complications, but 3D printing may hold the answer. “This is a new and exciting area of research in pharmaceutical sciences,” said Mansoor A. Khan, R.Ph., Ph.D., vice dean of the Texas A&M Health Science Center Irma Lerma Rangel College of Pharmacy in Bryan-College Station. The first drug made on a printer that was approved by the United States Food and Drug Administration (FDA) was for the geriatric population with epilepsy who—like children—can’t swallow large compressed pills easily.
“You really can get any amount of the drug that you want,” Khan said. “Imagine a pediatric patient whose dose depends on their body weight. Say they need a dose of 3.7 milligrams, but the drug manufacturers only make the medication as 25 milligram pills. So what do we do as pharmacists? We take the drug, crush it, put it in liquid and write out dosing instructions so that each teaspoonful or a defined dropper volume will contain 3.7 milligrams of active ingredient.” However, the drug might not be stable in the liquid form, so it might need to be kept in the refrigerator, or with the coating lost, the children might taste the bitterness of the drug.
Another issue is the formulation itself. Many tablets are specifically designed to be released over a period of time in specific segments of the gastrointestinal tract, and those benefits are lost if the drug is ground or crushed and put into liquid form.
Finally, there is relatively little quality control. Although the pharmacist is doing his or her best, of course, to err is human, and there is no system in place to test each formulation of the drug that each individual pharmacist has created for the pediatric patient. “We don’t need to validate each time because it’s going to an individual patient as a compounded product on a physician’s prescription order,” Khan said.
3D printing of specific, personalized doses could solve a number of these problems. “Each layer could be a tenth of a milligram. You want 0.9 milligrams? That’s nine layers. How about 3.7 milligrams? 37 layers,” Khan said. “You can even make them in the flavor that the kid wants.”
Continue reading on Vital Record.
This article by Christina Sumners originally appeared in Vital Record.